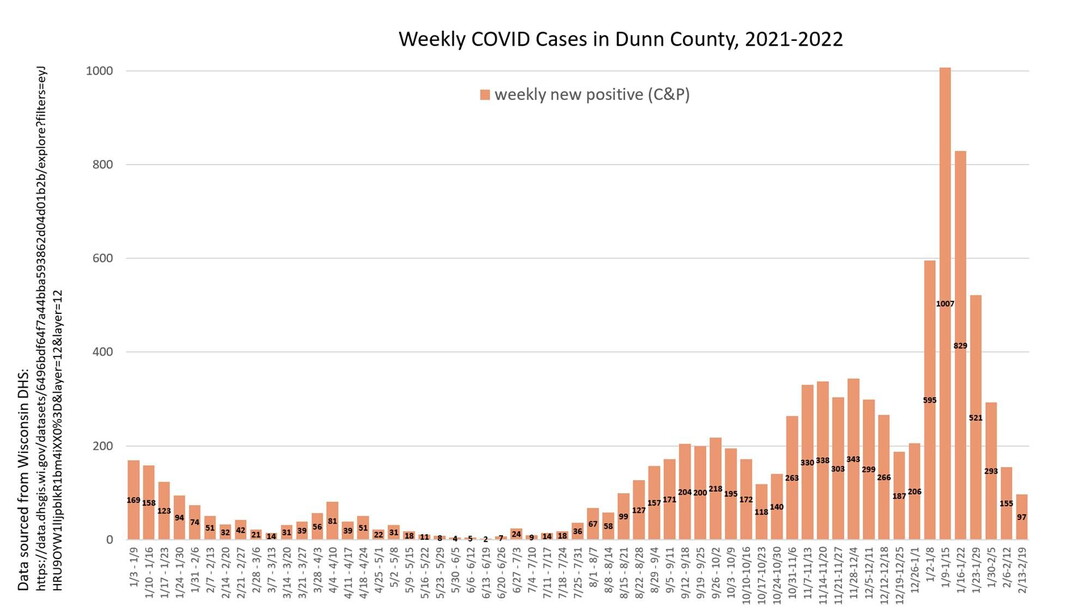
Weekly data update for Dunn County. Cases continue to fall, which is excellent news. Cases, hospitalizations, and ICU patients are at their lowest levels state-wide since August. Woo-hoo! That said, they are still HIGH. We had four more hospitalizations and another death in our county this past week. This tragedy is not yet ended. There is reason to be cautiously (always with this virus) optimistic, as percent positivity is way down to about 6% state-wide. This means that the decrease in cases is likely real and not due to under-testing or under-reporting of at-home tests (which we know are occurring). Therefore, cases will likely continue to decline; there is less virus circulating around and fewer vulnerable people who can catch it if exposed (a very high proportion of the population now has either infection-induced or vaccine-induced immunity or both). We will likely start to see more variability in case numbers week to week as numbers get lower, depending on if/when the virus finds its way to particular enclaves of vulnerable folks who haven't had it yet, be they vaccinated or not (it's still hunting for me - don't tell it where I am!). (Seriously, this is like the longest game of hide and seek I've ever played.) We may also plateau out at a lower but still high level as it continues to find those folks, but that will depend on luck as well as individual behaviors and events. We'll be able to infer that widespread community transmission is no longer occurring when case rates are even lower and when percent positivity is below 5% (and the lower the better), so we're not there yet.Good criticism of my previous estimate for Omicron case fatality rates led me to a different method - if you look at the curves of each wave, for both cases and deaths, you will see that they follow a very similar shape, usually offset by about one week. Comparing the peak average of daily deaths to the peak average of daily cases can give a fairly accurate picture, therefore, of the case fatality rate. When we do that for Omicron, we get a mortality rate of about 0.36%. This is about 1/4 the case fatality rate for previous variants of COVID but still more than 3x higher than the rate for influenza. The Omicron rate is likely to truly be lower than this, as we know that with this surge there are many more unreported cases (and thus a higher denominator) due to pandemic fatigue, less severe or absent symptoms in many, and the availability of at-home tests that don't get counted. But still, COVID is right now about 3-8x more prevalent than flu is during a typical flu season, so both that and the increased mortality rate make it reasonable to continue precautions.So, at present, the trends are looking good and hopeful that this spring will be one of relative calm COVID-wise. We're not there yet. And anything could happen. BUT if you haven't already, it's time to start thinking about how you'll make decisions about risk moving forward, as the landscape changes and shifts. At what point (if not already) will you feel safe gathering with a friend or friends? Will you have them test beforehand? How will you decide about going out to eat? Going to the gym? The answers will vary depending on your personal medical, infection, and vaccination history and risk tolerance, as well as the potential ramifications of having to miss work or, if you have young ones who are unvaccinated, having kids who will need to quarantine. Right now, I have a kid in the school musical who'd be mighty sore with me if I brought COVID home and infected them, forcing them to isolate and miss being in the show. So that's part of my current COVID-cautious stance. Edited to add: We still don't know what's going to happen with BA.2 here. So far, it hasn't done much. It's likely it will just expand the tail of our Omicron surge, but we'll see. https://www.npr.org/.../108.../omicron-ba2-variant-spread...
Support local news with a membership!
Alexandra Hall M.D. – Dr. Hall earned a Bachelor’s of Science in Science Education from New York University, taught high school in East Harlem, and then earned her M.D. from Mount Sinai School of Medicine.
She then completed a residency in Family Practice and served as Chief Resident at the University of Vermont. After practicing medicine for Dean Health System in Wisconsin and then at Cornell University in Ithaca, NY, Dr. Hall moved to Menomonie, WI to work at UW Stout, where she currently teaches for the Biology department and serves as a physician at Student Health Services.
Dr. Hall has a passion for educating people about health and science; she gives workshops regionally and nationally on various medical topics to both lay and professional audiences and has won several teaching awards for her work.


Add new comment